What is health? How do we measure the health of a society? Is it merely the clinical outputs of each individual patient or are these numbers impacted by environmental and social factors such as access to healthcare facilities? The answer is yes. Research surrounding health and social services shows a correlation between health outcomes and the environment, calling this junction the Social Determinants of Health (Bradley, et al., 2011; Bradley, et al., 2016; Woolf, et al., 2015). This includes a combination of factors that impact the health of an individual such as: access to food, income, education, physical activity, and proximity to care. This, in turn, impacts outcomes such as life expectancy and prevalence of disease. Reducing negative health outcomes has long-term, positive economic impacts. Healthcare costs related to preventable diseases, such as diabetes and obesity, could be reduced if individuals had access to resources that improve overall health. This improves the overall well-being of citizens; targeting such programs to vulnerable populations could have long term, positive impacts on community members’ health and the economy.
Access to Food and Physical ActivityFood deserts, in conjunction with lack of green space, contribute to limited options for healthy food choices and reduced physical activity among community members. USDA reports that the median percentage of Kentuckians with limited access to healthy foods is 3.47%. This number takes into account access to farmer’s markets, local grocery options, and is relatively low comparing the percentage to similar states. However, 31.45% of adults in Kentucky report “no leisure-time physical activity,” according to the CDC. This ranges between 20.5% in Fayette County to 40.1% of adults in Harlan County. The lack of physical activity may be partially attributed to limited access to exercise facilities.
*Source: County Health Rankings, 2016 |
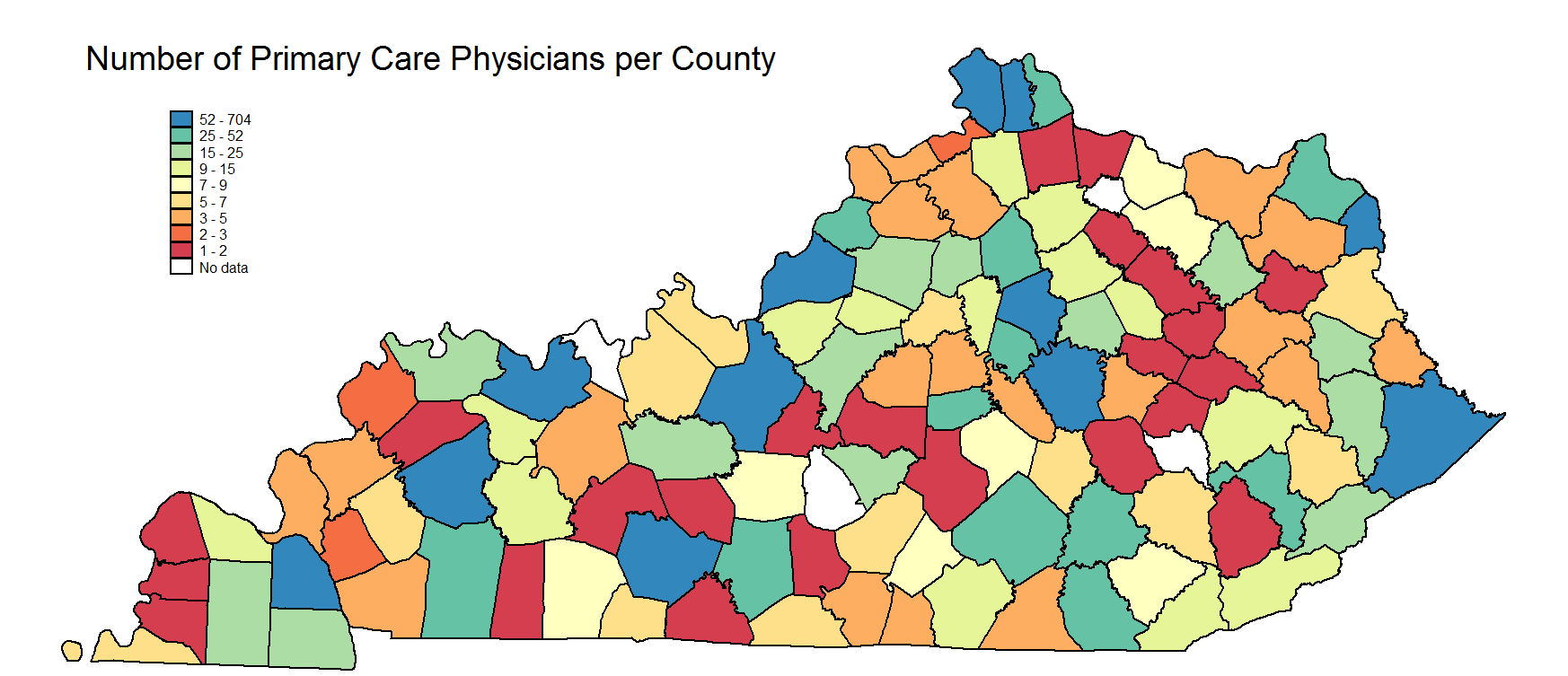
Proximity to HealthcareAccess to care contributes to a household’s ability to manage its overall health. If individuals can see a physician more frequently, they have greater opportunity to treat illnesses and utilize preventative care options. Forty-five counties in Kentucky have less than five primary care physicians, according to the County Health Rankings (2016).
*Source: County Health Rankings, 2016 |
||
Household IncomeAs income increases, prevalence of disease decreases and life expectancy increases. Individuals with lower incomes report higher incidence rates of heart disease, diabetes, dental decay, and obesity. Heart disease alone costs the Commonwealth of Kentucky approximately $280 billion per year, which includes health care expenditures and lost worker productivity.
|
Physical EnvironmentExposure to environmental pollution is higher among low income residents, which can have a negative impact on health. Air pollution negatively impacts health, in that it can lead to decreased lung function, chronic bronchitis, asthma, etc. One way to measure this is through the particulate matter found in the air, generated by combustion engines, forest fires, and power plants. Air is considered to be “good” if this number is between 1 and 12. In Kentucky, the overall average daily density is 13.5 micrograms per cubic meter, ranging between 12.9 and 14.6 (2014).
*Source: County Health Rankings, 2016 |
||
EducationCorrelated with income and race, education directly impacts employment. This in turn influences a household’s ability to cover health related expenses and utilize tools, such as health insurance for preventative care, which can be used to pay for annual examinations and vaccinations.
*Source: American Community Survey, 2014 |
For the complete 2016 Poster, click here.